Dangers of Infections: How to
Stay Safe
What is it and why is it important:
Infectious diseases are illnesses caused by harmful organisms (pathogens or
germs) that enter the body from outside. These germs include viruses, bacteria,
fungi and parasites. Such diseases affect people of all ages and range in severity
from mild illnesses to serious, life-threatening conditions. If not identified and
treated early, infections can lead to severe complications, permanent damage,
amputation or even death.
How Do We Get Infected:
Infections can spread in several ways, depending on the type of germ:
- Through Air: When an infected person coughs, sneezes, talks or even
breathes, tiny droplets or particles are released into the air. When others
inhale these, they could get sick. Examples include Flu (Influenza),
COVID-19 and Tuberculosis
- Through Direct Contact: Germs can spread by touching infected
people, wounds or contaminated surfaces and then touching your eyes,
nose or mouth. Examples include skin infections, diarrhoeal diseases,
Hepatitis B and C, HIV/AIDS and Flu (Influenza).
- Through Food or Water: Eating food or drinking water contaminated
with harmful bacteria, parasites, or viruses can cause infection. Examples:
Typhoid, Jaundice (Hepatitis A and E), Cholera.
- Through Vectors (Insect Bites): Some germs are carried by insects like
mosquitoes, fleas or ticks. When they bite, they can pass the infection to
humans. Examples include Malaria, Dengue and Chikungunya
- In Hospitals: Patients may get new infections while receiving treatment
in hospitals. These Hospital-Acquired Infections (HAIs) can happen
during surgeries, medical procedures or when using medical devices.
Infections can also spread through contact with other patients, healthcare
staff or contaminated surfaces and equipment. Examples include
Pneumonia (lung infection), bloodstream infections, wound infections,
urinary tract infections, etc.
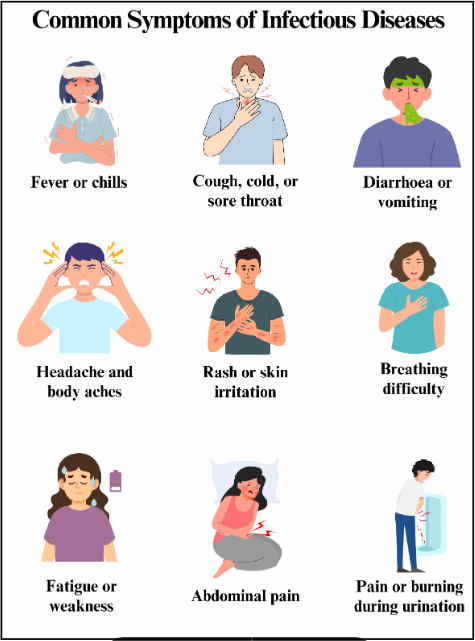
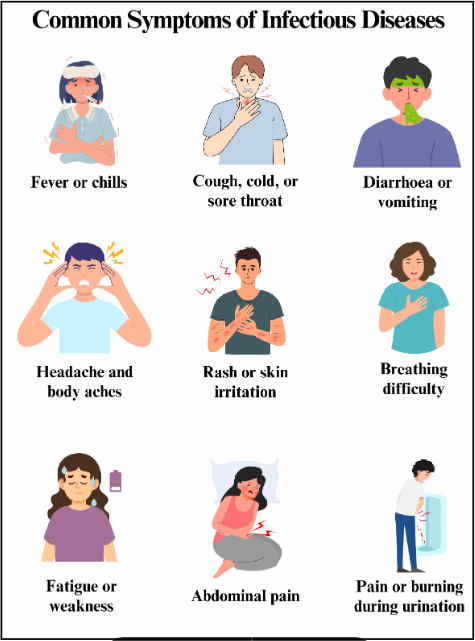
Symptoms of Infectious Diseases:
Symptoms vary with the type of infection and the organs affected. While some
people may have mild symptoms, others may fall seriously ill. Common signs
and symptoms may include one or more of the following:
Who is at Higher Risk:
While anyone can get an infection, some individuals are more susceptible and
have a higher risk of severe impact:
- The Young and Elderly: In infants and young children, immune systems
are not fully developed, and older people often have weakened immunity,
making it harder for their bodies to fight infections.
- People with Weak Immunity due to Diseases/Treatment: Those with
chronic diseases like diabetes, HIV or kidney problems and those
undergoing chemotherapy or organ transplants have a weakened immune
system.
- Patients in Hospitals: Hospitals have many sick people, which increases
the risk of the spread of germs through contact with air or medical staff.
Medical procedures such as surgeries, use of catheters, IV lines or
ventilators impact the body’s natural protective barriers, as they are
invasive and provide an easy pathway into the body.
- People with Open Wounds or Injuries: Cuts, burns or surgical wounds
provide an easy entry point for bacterial infections.
If infections are not identified and treated in time, they can be deadly. They can
spread quickly and can damage critical organs. Delayed treatment can even
cause death. If the symptoms persist even after common remedies, consult your
physician.
Diagnosis and Treatment:
The doctor will review your symptoms, medical history, and perform a physical
check-up and may prescribe some diagnostic tests like
- Blood tests to detect specific infections or pathogens
- Urine and stool tests for urinary or gastrointestinal infections
- Swabs from the throat, nose, wounds, and sputum samples
- X-rays and imaging to assess internal organs
- PCR, antigen tests, and fever panels for identifying viruses like COVID-
19, malaria, etc.
Accurate diagnosis is essential to identify the type and cause of infection, as the
treatment varies.
Treatment varies with the cause of the infection:
Treatments may include:
- Antibiotics: Effective against bacterial infections. Antibiotics do NOT
work against viruses.
- Antivirals: Used for specific viral infections like influenza, HIV, or
certain herpes viruses.
- Antifungals: For fungal infections.
- Supportive care: Such as oxygen, pain relief or fever control.
In severe or complicated cases, hospitalisation may be necessary for
monitoring and stabilising vitals.
Note: Self-medication or overuse of antibiotics can lead to harmful drug
resistance. Always follow the treatment prescribed by a doctor.
Preventing Infections:
Most infectious diseases are preventable with simple proactive measures by
individuals, families, communities and hospitals:
- Take recommended vaccines as per the schedule
- Wash your hands regularly, drink safe water and eat fresh, well-cooked
food. Wash fruits and vegetables properly before use. Avoid stale or
uncovered food.
- Protect yourself from mosquitoes by using nets, repellents and removing
stagnant water around the house
- Cover your mouth and nose while coughing or sneezing to stop spreading
infections to others
- Avoid close contact with people who are sick, and do not share personal
items like towels, razors or utensils
- Follow discharge instructions to avoid post-hospitalisation infections
Hospitals should contain infections:
- Implement strict hand hygiene protocols
- Follow sterilisation and disinfection practices
- Ensure staff training on infection control
- Use antibiotics responsibly (antimicrobial stewardship)
- Conduct routine surveillance and monitoring of infections
- Maintain isolation rooms for infected patients when needed
By understanding the basics of infections and proactively taking preventive
steps, you become an active partner in your healthcare journey, safeguarding
yourself. Your actions matter!